Understanding Gum Disease: What is Periodontitis and How Do I Fix It?

What is periodontitis (gum disease)?
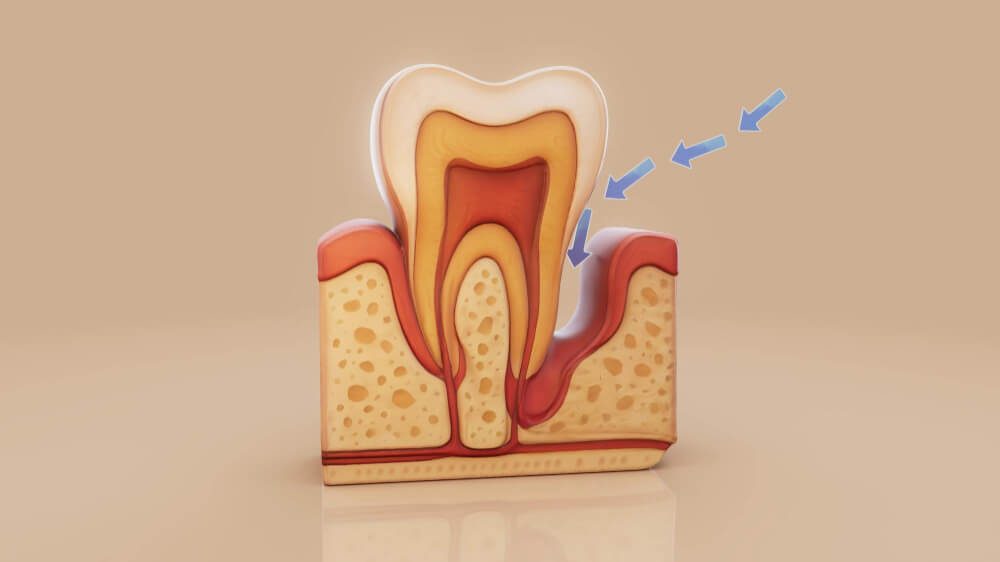
Periodontitis — commonly called gum disease — is an infection of the gums and bones that surround and support your teeth in the jaw bone. It usually starts as gingivitis (gum inflammation) caused by plaque and food deposits along the gumline of the teeth. If left unmanaged and untreated the inflammation spreads deeper and permanently destroys the connective tissues and bone that keep teeth stable in the jaw. Over time this can cause gum recession, deep “pockets” around teeth, loose teeth and tooth loss. This progression and the way clinicians describe it are well documented by dental authorities. Center for Disease Control and Prevention – Gum Disease
Quick fact: Periodontal disease is common — according to the Australian Institute of Health almost 1 in 3 adults (30% of people aged 15 and over) had moderate to severe periodontitis (gum disease) affects a significant portion of the population. Early detection is key.Australian Institute of Health
What causes gum disease (periodontitis)?
There can be many factors causing gum disease (periodontitis), but the primary cause is dental plaque — a sticky film of bacteria that accumulates along the gumline. It accumulates more quickly when there is food stuck on the tooth surface or between the gaps of the teeth. If plaque is not removed regularly it hardens like cement/plaster and turns into dental calculus (tartar) that can only be removed professionally. The bacteria and the body’s immune response to them cause inflammation that damages gum and bone.
Other important risk factors include:
- Smoking or vaping — strongly linked to worse periodontal disease and poorer outcomes. Periodontal Disease and Smoking: Systematic Review
- Diabetes — poorly controlled diabetes increases the risk and severity of periodontitis. Periodontal Diseases and Diabetes Mellitus: A Systematic Review
- Genetics / family history — some people are more susceptible. What Is the Heritability of Periodontitis? A Systematic Review
- Medicines and dry mouth — reduced saliva raises risk.
- Poor oral hygiene and irregular professional care.
How do dentists diagnose periodontitis?
Your dentist will diagnose gum disease by clinically looking inside your mouth to check for plaque, dental calculus, measure pocket depths and take x-rays. Diagnosis is both clinical and radiographic. Your dentist or hygienist will commonly:
- Measure pocket depths around each tooth with a periodontal probe (depths 3 mm can be a sign of gum disease).
- Check for bleeding on probing, gum recession, tooth mobility and signs of pus or inflammation.
- Take dental X-rays to look for bone loss around teeth.
- Use a staging/grading framework to describe severity and rate of progression (the modern staging & grading system helps guide treatment). PubMed Research Paper
Staging (I–IV) and grading (A–C) help dentists create a tailored treatment plan and predict future risk.
Common symptoms (what to watch for)
Periodontitis may be painless — that’s why it’s often missed. Look out for:
- Gums that bleed when you brush or floss.
- Red, swollen or tender gums.
- Gums pulling away from teeth (receding gums), making teeth look longer.
- Persistent bad breath or a bad taste.
- Teeth that feel loose or change position.
- Pus between teeth and gums or around a tooth.
If you notice any of these signs, book an exam with your dentist — early treatment keeps more of your natural teeth.Australian Dental Association Info Website

Evidence-based treatments: what works
Modern periodontal care uses a stepwise approach designed to control gum disease infection, reduce inflammation, stop disease progression and restore health where possible. The European Federation of Periodontology (EFP) S3-level guideline and other major bodies outline this staged approach.University of Dundee Research Journal
Stage 1 — Risk control & non-surgical therapy (first-line)
- Oral hygiene instruction (brushing technique, interdental cleaning).
- Professional cleaning (scaling and root planing, “deep cleaning”) to remove plaque and tartar from tooth surfaces and root surfaces. This is the backbone of non-surgical periodontal therapy and is recommended by the American Dental Association and clinical guidelines. American Dental Association Gum Disease Guidelines
- Adjunctive measures (antimicrobial mouthwashes, local antibiotics) may be recommended in specific situations based on your clinician’s assessment and the latest evidence. The choice of adjuncts is guided by clinical guidelines and individual patient needs.University of Dundee Research Journal
Stage 2 — Reassessment
After non-surgical therapy (often 4–12 weeks), your dentist will re-measure pockets and reassess inflammation. Many patients show significant improvement and can be maintained with regular professional cleans and strict home care.
Stage 3 — Surgical therapy (when needed)
If pockets remain deep or there is significant bone loss, surgical options may be offered:
- Flap surgery to access and clean roots and reduce pocket depths.
- Regenerative procedures (bone grafts, membranes, enamel matrix proteins) to try to restore lost bone and attach tissues in selected cases.
- Resective or plastic procedures to manage gum recession for function or aesthetics.
Clinical practice guidelines recommend surgery only when less invasive measures cannot adequately control the disease.University of Dundee Research Journal
Stage 4 — Maintenance
Long-term success depends on regular periodontal maintenance (3–6 monthly visits initially) and excellent daily home care. Without maintenance, recurrence is common. The EFP and national dental bodies emphasise ongoing maintenance as essential.
What about antibiotics or other adjuncts?
Systemic antibiotics are not routine for all periodontitis patients. They may be considered for specific aggressive or refractory cases or those with systemic risk factors — always under a dentist’s direction. Local antimicrobial agents (placed locally into pockets) can sometimes help as adjuncts to scaling and root planing. Evidence-based guidelines (EFP, ADA) recommend personalised use rather than routine blanket prescriptions. American Dental Association Gum Disease Non Surgical Approach
Periodontitis and general health — why it matters
Researchers have observed associations between periodontitis and systemic conditions such as diabetes and cardiovascular disease. While causality for many associations is still being studied, the link with diabetes is strong: better periodontal health can improve blood glucose control in some people. Public health bodies caution that more research is needed on causality, but they stress the importance of managing gum disease as part of whole-person health.
How My Local Dentists can help you (practical plan)
If you suspect gum disease or simply want to keep your gums healthy, here’s a practical 6-step plan you can follow — and what your dental team will do:
- Book an assessment — clinical exam and X-rays to check gum pocket depths and bone levels.
- Talk to your GP about managing your smoking and diabetes (if you smoke or have uncontrolled diabetes) — one of the best ways to protect your gums. We can point you to the right health professionals.
- Professional deep cleaning (scaling & root planing) and personalised oral hygiene coaching.
- Reassessment after 4–12 weeks to check response.
- Consider specialist periodontal referral if pockets remain deep or bone loss is advanced — surgical/regenerative options may be indicated.
- Long-term maintenance — ongoing hygiene visits and home care to prevent recurrence.
Our team at My Local Dentists works with you to build this plan, coordinate referrals where needed, and keep treatment comfortable and effective.
Prevention — everyday actions that really work
Preventing periodontitis is far easier than treating it. Key steps:
- Brush twice daily with a fluoride toothpaste using a soft toothbrush.
- Clean between teeth daily with floss, interdental brushes or water flossers (choose the tool that works for you).
- Visit your dentist regularly for check-ups and professional cleans.
- Stop smoking and control health conditions like diabetes.
- Eat a balanced diet and limit sugary snacks and acidic drinks.
National consumer resources (such as the Australian Dental Association’s patient guidance) recommend these same core steps for gum health. Australian Dental Association – Preventing Gum Disease
Costs and how long treatment takes
Treatment costs vary depending on severity, the number of visits, and whether surgical or specialist care is needed. Non-surgical therapy (scaling & root planing) usually takes a few appointments over several weeks; surgical treatments require additional time and healing. Your dentist can give a clear estimate after the initial assessment. Many Australian dental clinics offer payment plans or can refer you to public services where eligible.
FAQs — short answers to common questions
Q: Will I always lose teeth if I have periodontitis?
A: Not necessarily. With early diagnosis, effective treatment and ongoing maintenance many people keep their natural teeth. Advanced cases may require extraction of teeth that cannot be saved.
Q: Can I treat periodontitis at home?
A: Home care is essential, but professional treatment is needed to remove tartar and treat deep infection. Home care alone cannot reverse established bone loss.
Q: Are there ways to reverse bone loss?
A: Some regenerative procedures can rebuild bone in selected cases, but outcomes depend on individual factors. Prevention and early treatment remain the best strategy.
Evidence & references (selected)
The following organisations and research sources were used to ensure the blog reflects current, evidence-based guidance:
- American Dental Association (ADA) — Periodontitis overview and ADA resources on nonsurgical treatment and oral-systemic health. American Dental Association
- Australian Dental Association (ADA Australia) — consumer information, fact sheets and resources on gum health and periodontal disease (teeth.org.au / ADA pages). Australian Dental Association
- European Federation of Periodontology (EFP) — S3-level Clinical Practice Guideline: Treatment of stage I–III periodontitis (Sanz et al., 2020) — evidence-based stepwise treatment recommendations.University of Dundee Research Journal
- Tonetti et al., 2018 — Staging and grading framework for periodontitis used internationally for diagnosis and treatment planning. PubMed Research Article
- CDC / public health overviews — basic definitions and public health context for gum disease.Center for Disease and Control
Final words — take action today
Gum disease is common, often painless and yet preventable and treatable. If you’ve noticed bleeding gums, bad breath, gum recession or loose teeth — don’t ignore it. Early professional assessment and a personalised care plan from My Local Dentists will give you the best chance of stopping periodontitis in its tracks and keeping your smile for life.
Book an appointment with My Local Dentists today for a periodontal assessment, or call our clinic for advice on smoking cessation, diabetes management support and tailored oral hygiene instruction.
