The Impact of Smoking on Oral Health: A Comprehensive Overview

Introduction — why this matters to you
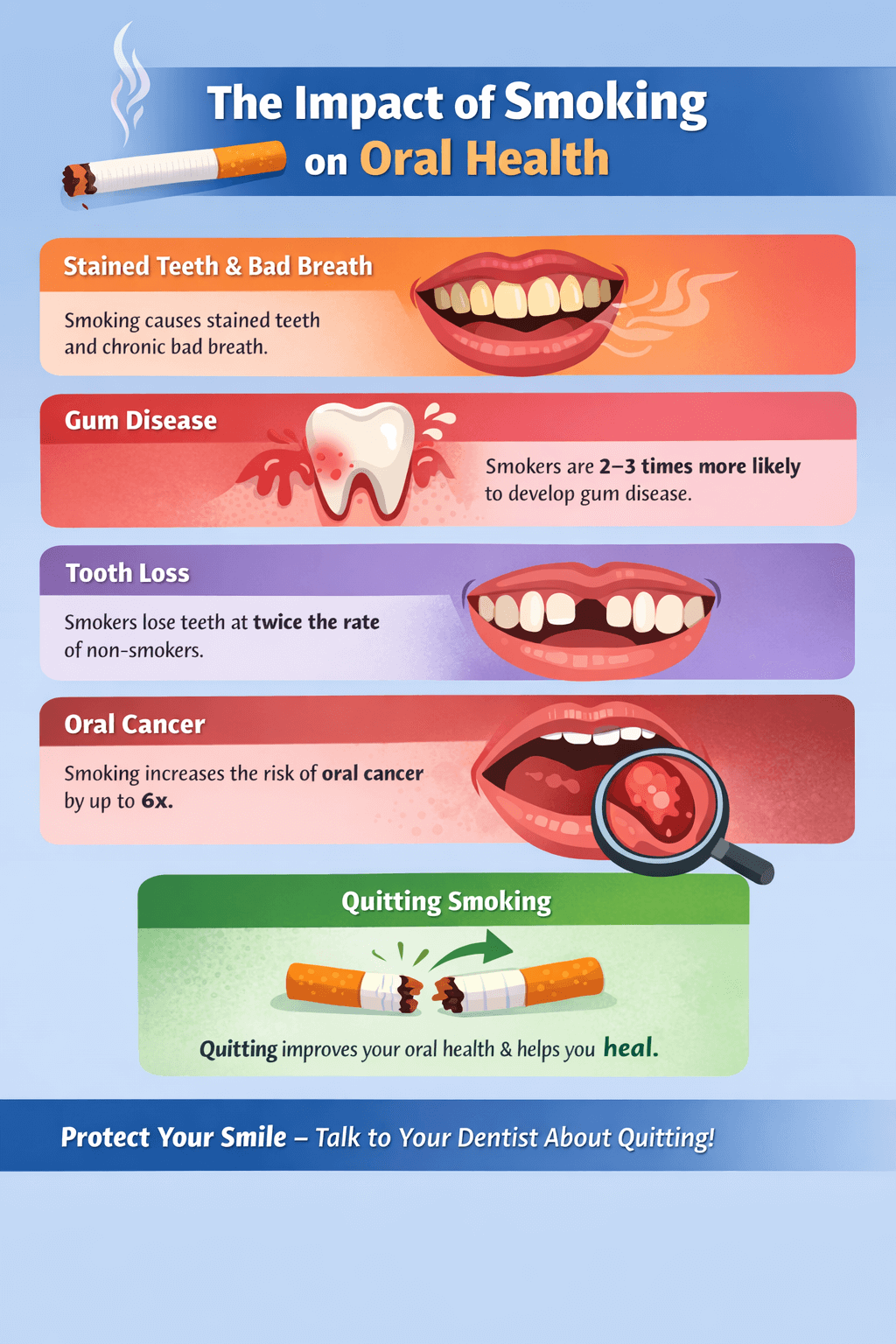
Smoking affects more than your lungs — it changes lots of different parts of your body including your mouth. From stained teeth and bad breath to gum disease, tooth loss and oral cancer, the damage is wide-ranging and well-documented behind many years of research. For anyone who smokes (or lives with someone who smokes), understanding these risks is the first step to protecting your smile — and your health. The Australian Dental Association and the American Dental Association both emphasise that dentists play a key role in identifying smoking-related oral disease and supporting patients to quit.
This article explains the evidence (using systematic reviews and major research where possible), how smoking causes oral problems, what to expect if you need dental treatment, and practical steps you can take — including quitting — to improve outcomes.
Quick facts — the headline risks of smoking for your mouth
- Smoking is a major cause of periodontitis (gum disease) and raises the chance of developing and progressing gum disease substantially.
- People who smoke are at much higher risk of oral cancer and precancerous mouth lesions than non-smokers. Combined use of alcohol and tobacco multiplies that risk.
- Dental implants are more likely to fail in smokers — some reviews report more than double the failure risk.
- Smoking also causes tooth staining, bad breath, delayed healing after dental treatments, and higher chances of tooth loss.
These are not minor annoyances — they affect your quality of life, the success of dental care, and in the case of oral cancer, can threaten life itself.
How smoking damages the mouth — the biology in plain language
Smoking introduces thousands of chemicals into your mouth — nicotine, tar, carbon monoxide and many carcinogens. These have three broad harmful effects:
- Direct tissue damage and carcinogenesis. Chemical exposure damages the cells lining your mouth, increases mutations and raises the risk of oral cancer and precancerous lesions. Alcohol and tobacco together have a synergistic effect, making cancer risk especially high for people who both drink and smoke.
- Immune suppression and altered blood flow. Nicotine and other compounds reduce blood flow to gum tissues and suppress the immune system. Imagine wanting to water the garden with a hose but finding out that the garden hose is damaged or kinked or has holes in it. Reduced blood flow and a suppressed immune system makes it harder for your gums to fight infection and for wounds to heal in general from existing plaque and germs inside the mouth but especially after surgery or dental procedures. Reduced blood flow also masks signs of gum disease — smokers often don’t show the same gum redness and bleeding that non-smokers do, which can delay diagnosis and hide the severity of the problem.
- Changes to oral bacteria and plaque behaviour. Smoking alters the mouth’s bacterial ecosystem, encouraging harmful species associated with gum disease and making plaque more destructive. These bacterial changes, combined with impaired immunity, accelerate periodontal breakdown (gum and bone loss). Systematic reviews report substantially higher rates of periodontitis in smokers compared with non-smokers.
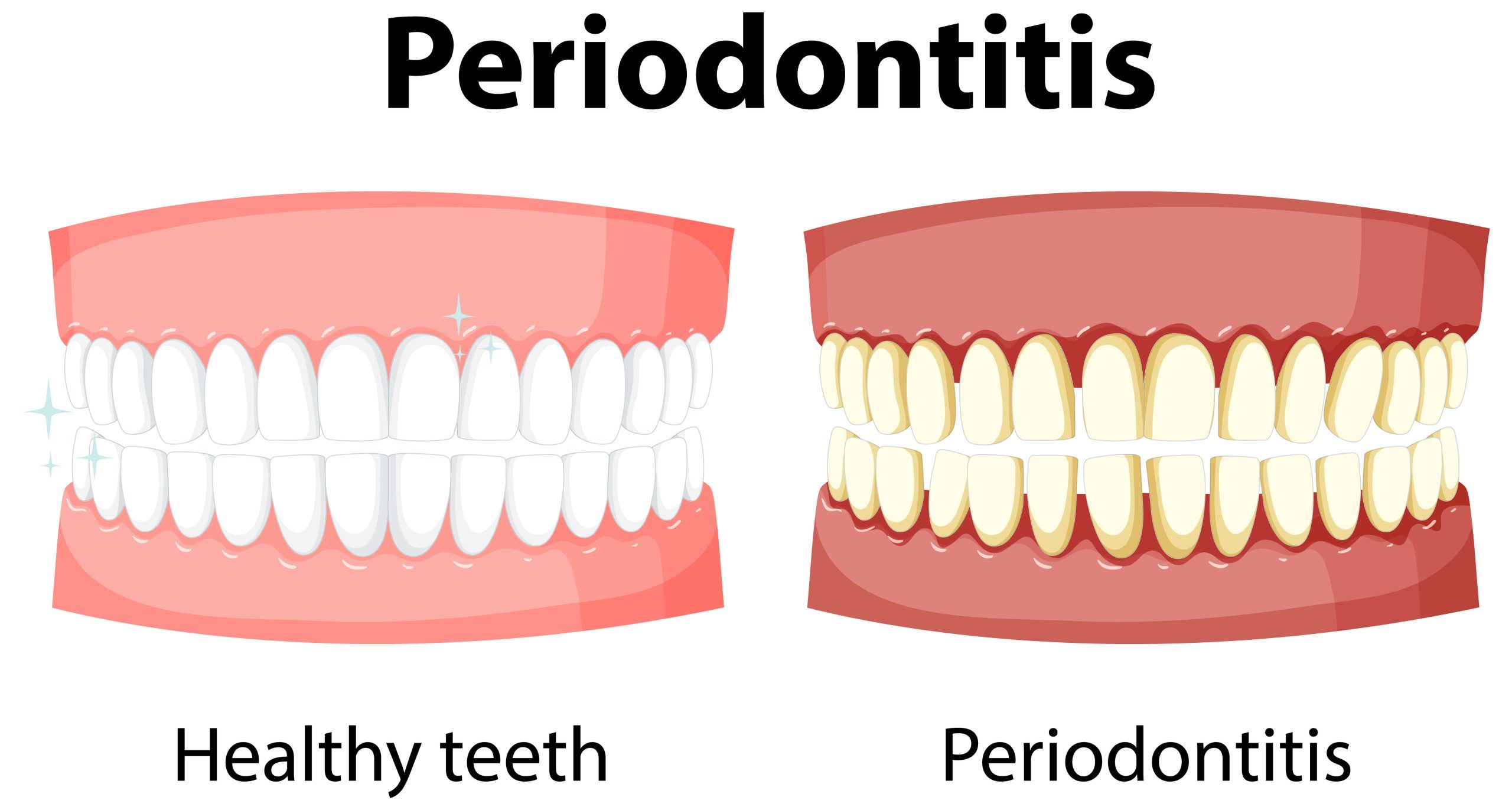
Smoking and gum disease (periodontitis): what the evidence says
Periodontitis is an infection of the gums and bones that hold the teeth in the jawbone. It is an infection-driven inflammation that destroys the gums, periodontal ligament and jaw bone supporting the teeth leading to pain, bone loss, loose teeth, sensitive teeth and ultimately tooth loss. High-quality studies and systematic reviews have consistently shown that current smoking significantly increases the risk of developing and progressing periodontitis. A pooled analysis in recent systematic reviews estimated a substantially higher risk (some meta-analyses report around an 80–85% higher risk for current smokers versus never-smokers). In public health terms, a sizeable portion of periodontitis cases is attributable to smoking.
Why this matters in practice:
- Smokers experience faster attachment and bone loss around teeth.
- Gum disease in smokers is more likely to be severe and less responsive to therapy unless smoking stops.
- Even after professional periodontal treatment, smokers tend to have poorer outcomes and higher relapse rates compared with non-smokers.
For dental procedures, this means: if you smoke, your treatment plan and prognosis will differ to patients who don’t smoke — and quitting will improve long-term results.
Smoking and oral cancer: the facts
Tobacco smoking is a primary risk factor for cancers of the mouth, tongue, floor of mouth, and throat. Meta-analyses and long-term epidemiological studies demonstrate a strong dose–response relationship: heavier and longer smoking leads to higher cancer risk. The combination of smoking and alcohol multiplies the risk further. Public health authorities in Australia and internationally classify tobacco as a causal agent for oral cancers.
Key takeaway: smoking increases the risk of getting oral cancer, and quitting reduces risk over time — another powerful reason to stop.
Smoking and dental treatment outcomes (implants, extractions, healing)
Smoking doesn’t just cause disease — it makes dental care more complicated:
- Dental implants: Systematic reviews have found that implants placed in smokers have a significantly higher failure rate than implants in non-smokers (often more than double the risk). Smokers are also more likely to develop peri-implantitis (infection around implants). If you’re considering implants, your dentist will discuss how smoking increases your risk of failure and may recommend quitting before and after the procedure to improve success.
- Surgery & healing: Smoking delays wound healing after extractions, periodontal surgeries and other oral surgeries. This can increase complications such as infection, dry socket and poor bone healing.
- Restorations & cosmetics: Teeth stained by smoking may not respond as well to whitening treatments, and continued smoking will quickly re-stain treated teeth. Prosthetic work may also be affected by tissue changes and hygiene challenges.
Secondhand smoke and oral health
You don’t have to be a smoker yourself to be at risk. Systematic reviews report that exposure to secondhand smoke is associated with an increased risk of oral cancer and can affect children’s oral health (higher caries risk, for example). Protecting children and family members from smoke exposure is part of overall oral cancer and dental disease prevention.
What happens when you quit? — the benefits for your mouth
Quitting smoking produces clear oral health benefits, some of which begin quickly:
- Improved blood flow and healing: Within weeks to months, tissue blood flow and wound-healing capacity improve, helping after surgery or periodontal therapy.
- Lowered risk over time: The risk of oral cancer begins to fall after quitting and continues to decrease with longer abstinence.
- Better treatment outcomes: Periodontal therapy, implant success and general dental treatment outcomes improve if a patient quits smoking before and after procedures.
- Appearance & breath: Staining gradually reduces (with professional help), and halitosis (bad breath) improves over time.
Even if you’ve smoked for years, quitting helps. Dental teams are well-placed to provide brief advice, motivational support and referrals to cessation services such as Quitline — and this assistance improves quit rates. The Australian Dental Association encourages dentists and patients to talk openly about this topic and to help support patients who want to stop.
How My Local Dentists approaches patients who smoke
We know quitting is hard. At My Local Dentists we follow an evidence-based, supportive approach:
- Routine screening — we ask about tobacco and vaping at new-patient checks and routine exams.
- Oral cancer checks — smokers receive careful soft-tissue exams and are photographed and monitored for suspicious lesions.
- Clear communication — we explain how smoking affects diagnosis, treatment options and expected outcomes.
- Cessation support — we offer brief interventions, tailored advice, and referrals to Quitline or GP services for pharmacotherapy (e.g., nicotine replacement therapy or prescription medications).
- Treatment planning — for smokers needing periodontal therapy, implants or oral surgery, we include smoking-related risks in consent discussions and recommend quitting before surgery to improve healing.
Our goal is non-judgmental help: better dental outcomes and better overall health.
Practical steps for smokers — what you can do right now
- Book a dental check-up — tell us if you smoke so we can screen for early problems. Early detection makes treatment simpler and cheaper.
- Get a professional clean and oral cancer check — regular hygiene visits reduce plaque, tartar and inflammation and let us detect suspicious lesions early.
- Talk to us about quitting — even short counseling from the dental team increases the chance you’ll try to quit. We can connect you with Quitline and medical supports.
- If you’re planning implants or surgery, plan your quit date — stopping before and after surgery improves outcomes. Your dentist will advise a safe timeline.
- Protect household members — avoid smoking around children and family to reduce their risk of oral health problems.
Common questions patients ask
Q: I don’t have pain — do I still need to worry?
A: Yes. Smoking can mask the symptoms of gum disease (less bleeding and redness), so silent damage can be occurring. Regular dental exams are essential.
Q: I vape instead of smoking — is it safer for my mouth?
A: Vaping may carry fewer of some of the toxicants in cigarette smoke, but evidence is still emerging and vaping can also affect gum health, taste and healing. Tell your dentist if you vape so we can monitor you closely.
Q: Will quitting reverse the damage?
A: Quitting helps healing and lowers future risks, but some damage (like advanced gum bone loss or existing cancer) may not be fully reversible. That’s why early quitting and early dental care matter.
Final message — why act today
Smoking causes many oral problems — from stained teeth and bad breath to serious diseases like periodontitis and oral cancer. It also makes dental treatment more difficult and less predictable. The good news: quitting helps, and dental teams can support you through both prevention and treatment.
If you smoke, don’t wait for the symptoms to appear. Book a check-up with My Local Dentists today for a full oral health assessment, an oral cancer check, and friendly support to plan your next steps — including quitting if you’re ready. Your mouth (and your whole body) will thank you.
Source References for Further Information
Australian Dental Association (ADA Australia)
- Australian Dental Association. Smoking and Oral Health.
https://www.teeth.org.au/smoking-and-oral-health
- Australian Dental Association. Oral Cancer – What You Need to Know.
https://www.teeth.org.au/oral-cancer
- Australian Dental Association. Gum Disease (Periodontal Disease).
https://www.teeth.org.au/gum-disease
American Dental Association (ADA – USA)
- American Dental Association. Smoking, Tobacco Use & Oral Health.
https://www.ada.org/resources/ada-library/oral-health-topics/smoking-and-oral-health
- American Dental Association. Periodontal (Gum) Disease.
https://www.ada.org/resources/ada-library/oral-health-topics/periodontal-disease
- American Dental Association. Oral Cancer.
https://www.ada.org/resources/ada-library/oral-health-topics/oral-cancer
High-Quality Research (Systematic Reviews & Major Studies)
- Leite FRM, Nascimento GG, Scheutz F, López R.
Effect of smoking on periodontitis: A systematic review and meta-regression.
Journal of Dental Research. 2018.
https://journals.sagepub.com/doi/10.1177/0022034518780430
- Nociti FH Jr, Casati MZ, Duarte PM.
Current perspective of the impact of smoking on the progression and treatment of periodontitis.
Periodontology 2000. 2015.
https://onlinelibrary.wiley.com/doi/10.1111/prd.12063
- Warnakulasuriya S.
Global epidemiology of oral and oropharyngeal cancer.
Oral Oncology. 2009.
https://www.sciencedirect.com/science/article/pii/S1368837509001804
- Heitz-Mayfield LJA, Huynh-Ba G.
History of treated periodontitis and smoking as risks for implant therapy.
Clinical Oral Implants Research. 2009.
https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0501.2009.01784.x
- Chrcanovic BR, Albrektsson T, Wennerberg A.
Smoking and dental implants: A systematic review and meta-analysis.
Journal of Dentistry. 2015.
https://www.sciencedirect.com/science/article/pii/S0300571215001408
- US Surgeon General.
The Health Consequences of Smoking—50 Years of Progress.
https://www.ncbi.nlm.nih.gov/books/NBK179276/
Second-Hand Smoke & Oral Health
- Aligne CA, Moss ME, Auinger P, Weitzman M.
Association of secondhand smoke exposure with dental caries in children.
Pediatrics. 2003.
https://publications.aap.org/pediatrics/article/112/4/e404/64806
